Understanding When to Consult a Urologist
What are the top signs that you should see a urologist in NYC? The urinary tract and male reproductive system are crucial to overall health, yet many individuals put off seeing a urologist until symptoms become severe. In a city as fast-paced as New York, it’s easy to ignore signs that could point to urological conditions—but early detection can make a world of difference. If you’re wondering when to make an appointment with a urologist in NYC, here are the top signs to watch for.

1. Frequent or Painful Urination
Experiencing pain, burning sensations, or an urgent need to urinate often may be signs of a urinary tract infection (UTI), bladder inflammation, or even more serious conditions like interstitial cystitis. While UTIs are more common in women, men who develop them should seek evaluation from a urologist, as they can indicate underlying issues like prostatitis or urinary blockages.
2. Blood in Urine (Hematuria)
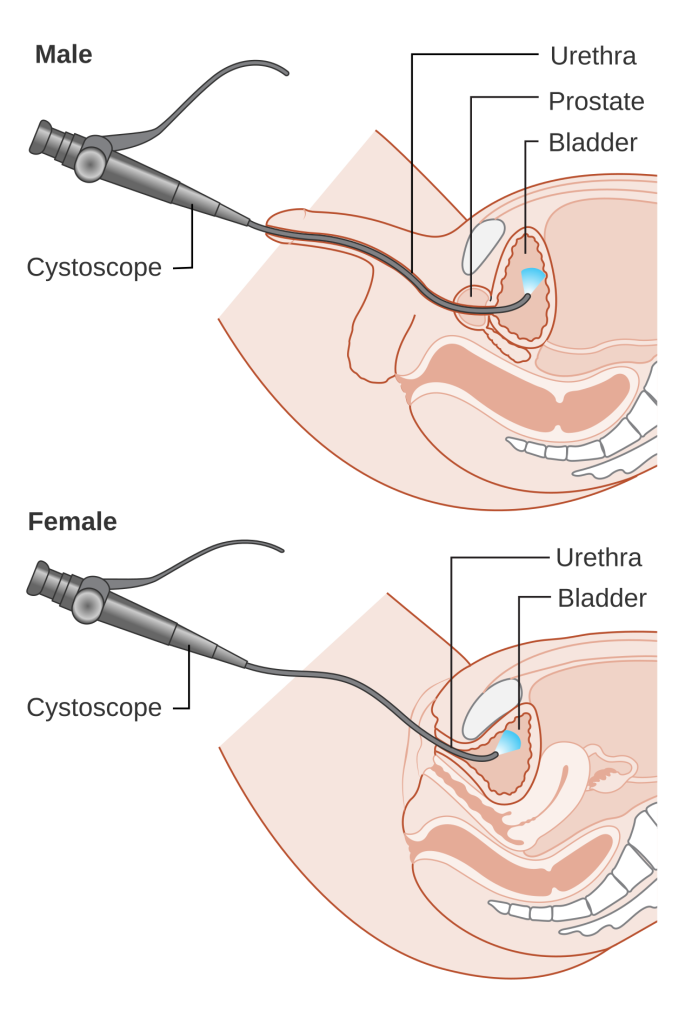
Seeing blood in your urine is never normal and should prompt immediate medical attention. This symptom can be caused by kidney stones, infections, or in some cases, urological cancers such as bladder or kidney cancer. A urologist will perform diagnostic tests, such as a cystoscopy or imaging, to determine the source.
3. Erectile Dysfunction (ED)
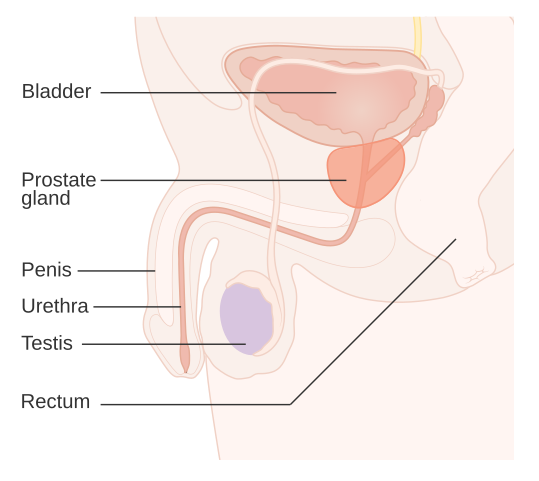
While many men may feel embarrassed to discuss erectile dysfunction, it’s a common condition that urologists regularly treat. ED can be a symptom of hormonal imbalances, cardiovascular disease, or prostate issues. New York urologists offer advanced therapies for ED, including medications, injections, and penile implants.
4. Male Infertility
If you and your partner have been trying to conceive for over a year without success, a urologist can help identify and treat male-factor infertility. Conditions like varicoceles, hormonal imbalances, or blockages can often be corrected, restoring fertility and improving reproductive outcomes.
5. Testicular Pain or Mass
Any lump, swelling, or persistent pain in the testicles should be evaluated by a urologist. These could be signs of infection, cysts, or in some cases, testicular cancer. Early diagnosis and treatment greatly improve outcomes for such conditions.
6. Incontinence or Difficulty Controlling Urine
Urinary incontinence affects both men and women and can significantly impact quality of life. Whether it’s stress incontinence, urge incontinence, or overflow, a urologist can perform specialized evaluations to determine the cause and suggest treatments ranging from pelvic floor therapy to surgery.
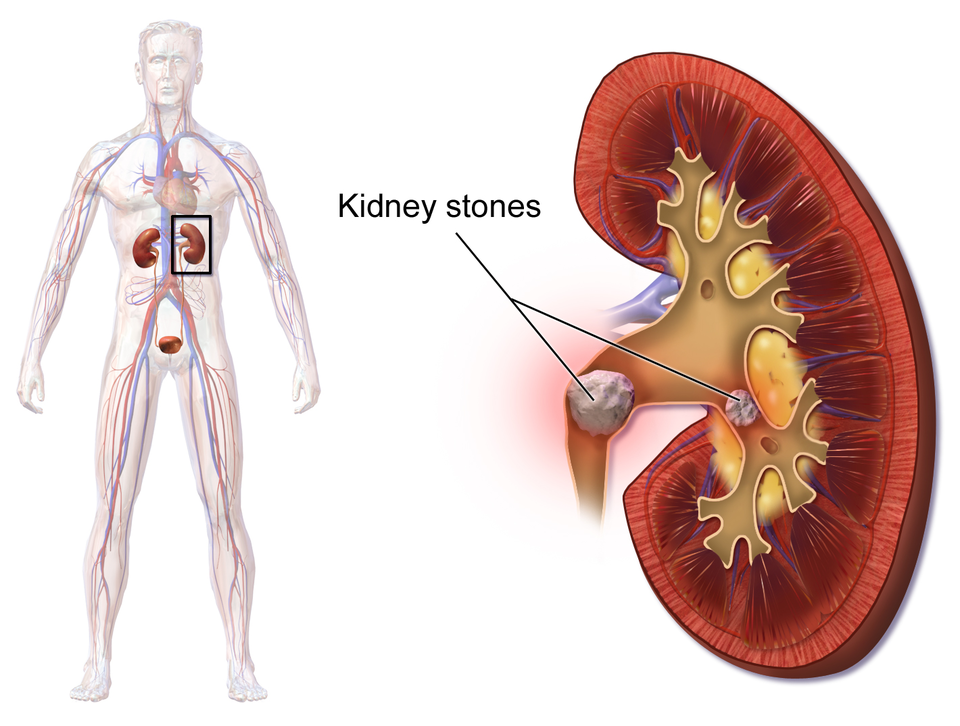
7. Kidney Stones
If you’ve ever had a kidney stone, you know how painful it can be. Symptoms include severe side or back pain, nausea, and blood in urine. A urologist can help manage and prevent future stone formation through dietary guidance and medical therapies.
8. Abnormal Prostate Test Results
Men over 50—or earlier if at high risk—should undergo routine prostate exams. If you’ve had abnormal PSA (prostate-specific antigen) levels or felt a lump during a digital rectal exam (DRE), a urologist can investigate further to rule out prostate cancer or other disorders.
9. Pain in the Lower Abdomen or Pelvis
Chronic or unexplained pelvic pain could be related to the bladder, prostate, or reproductive organs. A urologist will conduct appropriate tests to find the underlying cause and create a personalized treatment plan.
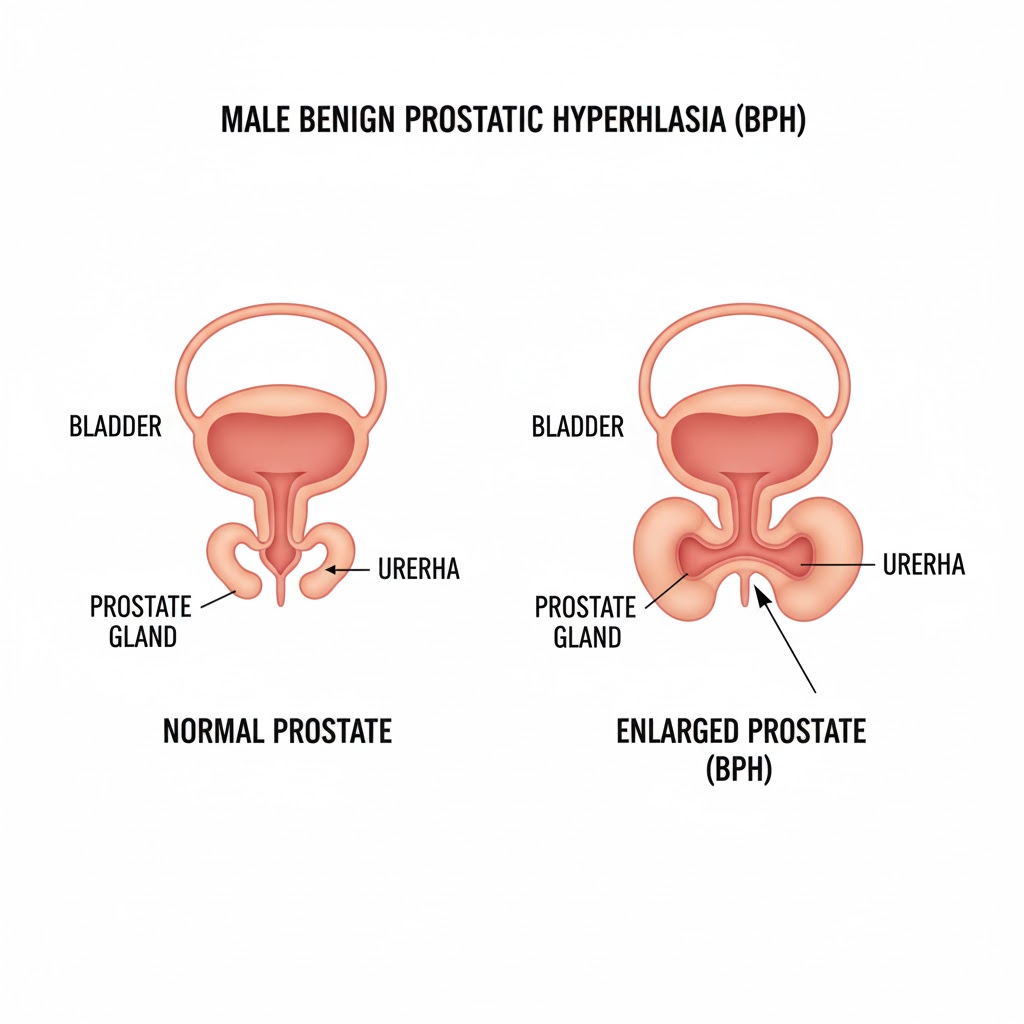
10. Changes in Urine Stream or Bladder Function
Slow urine flow, dribbling, or straining to urinate may signal benign prostatic hyperplasia (BPH) or urethral stricture. Both conditions can be treated with medication or minimally invasive procedures offered by skilled NYC urologists.
Top Signs You Should See a Urologist in NYC: Conclusion
If you’re experiencing any of the symptoms mentioned above, don’t wait. Early intervention by a qualified urologist can significantly improve your health outcomes and quality of life. Living in NYC gives you access to some of the best urological care in the country—use it to your advantage.
Looking for Expert Urological Care in NYC?
At Fifth Avenue Urology, Dr. Yaniv Larish offers compassionate, expert care for a wide range of urological issues, from kidney stones to prostate health, male infertility, and more. With cutting-edge diagnostic tools and personalized treatment plans, Dr. Larish is one of NYC’s trusted urology specialists for both men and women.
FIFTH AVENUE UROLOGY
Dr. Yaniv Larish
4 East 76th Street
New York, NY 10021
212-675-3186
Schedule a consultation today and take the first step toward better urological health.
 Dr. Larish is a urologist and surgeon treating women and men with a variety of urological conditions. His expertise is in treating complex kidney stones, enlarged prostates (BPH), incontinence, erectile dysfunction, infertility, and urological oncology (prostate, bladder, kidney, and adrenal cancers). He is an expert in general urology and is often consulted for second opinions.
Dr. Larish is a urologist and surgeon treating women and men with a variety of urological conditions. His expertise is in treating complex kidney stones, enlarged prostates (BPH), incontinence, erectile dysfunction, infertility, and urological oncology (prostate, bladder, kidney, and adrenal cancers). He is an expert in general urology and is often consulted for second opinions.